
hip Resurfacing
Disclaimer: This information is an educational resource only and should not be used to make a decision on hip resurfacing or about arthritis management. All decisions about total hip resurfacing or about arthritis management must be made in conjunction with your surgeon or a licensed healthcare provider.
Introduction to Hip resurfacing
Patients with advanced arthritis of the hip may be candidates for either traditional total hip replacement (arthroplasty) or hip resurfacing (hip resurfacing arthroplasty).
Each of these procedures is a type of hip replacement, but there are important differences.
Dr Bhimani will talk with you about the different procedures and which operation would be best for you.
DESCRIPTION
In a traditional total hip replacement, the head of the thighbone (femoral head) and the damaged socket (acetabulum) are both removed and replaced with metal, plastic, or ceramic components.
In hip resurfacing, the femoral head is not removed, but is instead trimmed and capped with a smooth metal covering. The damaged bone and cartilage within the socket is removed and replaced with a metal shell, just as in a traditional total hip replacement.
Front Of A Healthy HIp

The hip is a ball and socket joint. In a healthy hip, the bones are covered with smooth cartilage that enables the femoral head and acetabulum to glide painlessly against each other.
Advantages of Hip resurfacing
The advantages of hip resurfacing over traditional total hip replacements is an area of controversy among orthopaedic surgeons, and Dr Bhimani will discuss with you’re the pros and cons of each option based on your condition and requirements.
Hip Resurfacing May Be Easier To Revise
Because the components (called implants) used in hip replacements and hip resurfacing are mechanical parts, they can — and do — wear out or loosen over time. This typically occurs between 10 and 20 years after the procedure, although implants may last longer or shorter periods of time.
If an implant fails, an additional operation may be necessary. This second procedure is called a revision and it can be more complicated than the initial operation. Because hip resurfacing removes less bone from the femur (thighbone) than a traditional hip replacement, many surgeons believe it is easier to exchange implants that fail after hip resurfacing.
Decreased Risk of Hip Dislocation
In hip resurfacing, the size of the ball is larger than in a traditional hip replacement, and it is closer to the size of the natural ball of your hip. Because of this, it may be harder to dislocate. This stance is controversial because several factors can affect the risk of dislocation, such as surgical approach, and the type and size of the implants used.
More Normal Walking Pattern
Several studies have shown that walking patterns are more natural following hip resurfacing compared to traditional hip replacement. These differences in walking are quite subtle, however, and special instruments are needed to measure them.
Hip Osteoarthritis

DISAdvantages of Hip resurfacing
Femoral Neck Fracture
A small percentage of hip resurfacing patients will eventually break (fracture) the thighbone at the femoral neck. If this occurs, it is usually necessary to convert the hip resurfacing into a traditional hip replacement.
A femoral neck fracture is not possible with a traditional hip replacement because the femoral neck is removed during this procedure. However, fractures around the implants can still occur with a traditional hip replacement.
Metal Ion Risk
In hip resurfacing, a metal ball moves within a metal socket. Over time, this leads to the production of tiny metal particles called ions. Some patients may develop sensitivity or allergy to the metal particles, which may cause pain and swelling. Also, there are concerns that the metal particles may increase the risk of cancer, although this has never been proven. Some types of traditional hip replacements also consist of a metal ball and a metal socket and these replacements run the same potential risks.
Hip Resurfacing Is A More Difficult Operation
resurfacing Hip are more difficult than total hip replacements for surgeons to perform. As such, a larger incision is usually required for a hip resurfacing.
Healthy vs arthritic hip
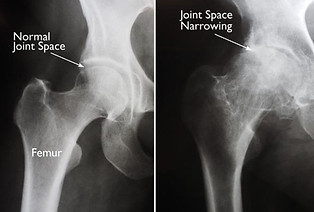
(Left) In this x-ray of a normal hip, the space between the ball and socket indicates healthy cartilage. (Right) This x-ray of an arthritic hip shows severe loss of joint space.
CANDIDATES FOR SURGERY
Dr Bhimani may recommend surgery if you have more advanced osteoarthritis and have exhausted the nonsurgical treatment options.
Surgery should only be considered if your hip is significantly affecting the quality of your life and interfering with your normal activities.
Unlike hip replacement, hip resurfacing is not suitable for all patients. Generally speaking, the best candidates for hip resurfacing are younger (less than 60), larger-framed patients (often, but not always male) with strong, healthy bone.
Patients that are older, female, smaller-framed, with weaker or damaged bone are at higher risk of complications, such as femoral neck fracture.
A comprehensive evaluation by Dr Bhimani will help you determine if you are a good candidate for hip resurfacing.
Blood Clots

Blood clots may form in one of the deep veins of the body. While blood clots can occur in any deep vein, they most commonly form in the veins of the pelvis , calf or thigh
YOUR SURGERY
Before Surgery
You will likely be admitted to the hospital on the day of surgery.
Before your procedure, a doctor from the anesthesia department will evaluate you. He or she will review your medical history and discuss anesthesia choices with you.
You should also have discussed anesthesia choices with Dr Bhimani during your preoperative clinic visits. Anesthesia can be either general (you are put to sleep) or spinal (you are awake but your body is numb from the waist down).
Surgical Procedure
A hip resurfacing operation typically lasts between 1 1/2 and 3 hours.
Dr Bhimani will make an incision in your thigh in order to reach the hip joint. The femoral head is then dislocated out of the socket. Next, the head is trimmed with specially designed power instruments. A metal cap is cemented over the prepared femoral head.
The cartilage that lines the socket is removed with a power tool called a reamer. A metal cup is then pushed into the socket and held in place by friction between the bone and the metal.
Once the cup is in place, the femoral head is relocated back into the socket and the incision is closed.
After the surgery you will be taken to the recovery room, where you will be closely monitored by nurses as you recover from the anesthesia. You will then be taken to your hospital room.
Hip Resurfacing X-Ray

(Left) In the x-ray of a hip resurfacing taken from the front, a metal cap now covers the femoral head, and a small stem is seen in the femoral neck. A metal socket is also in place. Unlike the traditional total hip replacement shown on the right, the femoral head and the neck are not removed.
COMPLICATIONS
As with any surgical procedure, there are risks involved with hip resurfacing. Dr Bhimani will discuss each of the risks with you and will take specific measures to help avoid potential complications.
Although rare, the most common complications of hip resurfacing are:
Blood Clots
Blood clots in the leg veins are the most common complication of hip resurfacing surgery. Blood clots can form in the deep veins of the legs or pelvis after surgery. Blood thinners such as warfarin (Coumadin), low-molecular-weight heparin, aspirin, or other drugs can help prevent this problem.
Infection
You will be given antibiotics before the start of your surgery and these will be continued for about 24 hours afterward to prevent infection.
Injury to nerves or vessels
Although it rarely happens, nerves or blood vessels may be injured or stretched during the procedure.
Femoral neck fracture
Dislocation
Risks of anesthesia
RECOVERY
In most cases, patients go home 1 to 4 days after surgery.
You may begin putting weight on your leg immediately after surgery, depending on Dr Bhimani’s preferences and the strength of your bone. You may need a walker, cane, or crutches for the first few days or weeks until you become comfortable enough to walk without assistance.
You can expect some pain and discomfort for at least a week after surgery. Dr Bhimani may prescribe pain medicine, if needed.
Many types of pain medication are available to help control pain, including opioids, nonsteroidal anti-inflammatory drugs (NSAIDs) and local anesthetics.
Treating pain with medications can help you feel more comfortable, which will help your body heal faster and recover from surgery faster.
A physical therapist will give you exercises to help maintain your range of motion and restore your strength. You will continue to see
Dr Bhimani for follow-up visits in his or her clinic at regular intervals.
You will most likely resume your regular activities of daily living by 6 weeks after surgery.
OUTCOME
The vast majority of Dr Bhimani’s patients who undergo a hip resurfacing experience favourable long-term outcomes including relief from pain and increased stability and function. Complete pain relief and restoration of function is not always achievable and patients may still experience pain or knee stiffness.
Surgery is not a pleasant prospect for anyone, but for some people with arthritis, it could mean the difference between leading a happier normal life or putting up with a debilitating pain and immobility.
Dr Bhimani believes that surgery should only be undertaken once non-operative treatment has failed, and that the decision to have surgery should be a considered one.
Although most people are extremely happy following surgery, complications can occur. It is important you understand these potential complications and if you have any questions to speak with Dr Bhimani.
If you are undecided, it is best to wait until you are sure this is the procedure for you.
